Table of Contents
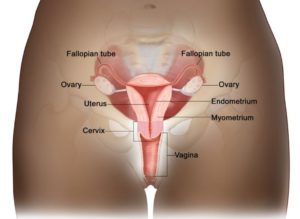
What is Cervical Cancer?
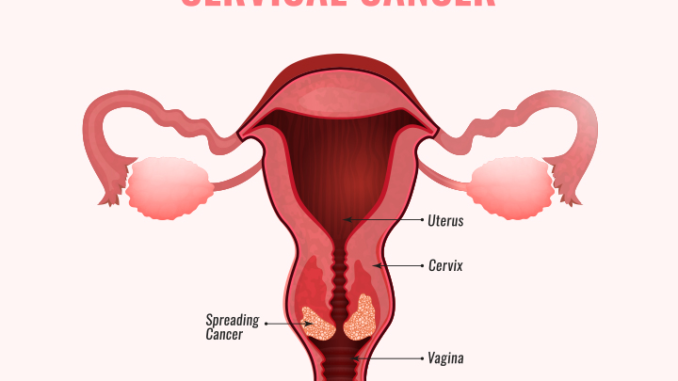
- Cervical cancer is the development or growth of abnormal cells in the lining of the cervix.
- Cervical cancer is the cancer that occurs in the cells of the cervix- the lower portion of the uterus that attaches to the vagina.
- The most common cause of cervical cancer is Human Papilloma Virus (HPV). HPV accounts large majority (95%) of cervical cancer.
- Squamous cell carcinoma is the most common type of cervical cancer.
- Before cancer develops in the cervix, the cervical tissue undergoes changes known as dysplasia, in which abnormal cells start to emerge in the tissue.
- If left unchecked or untreated, these abnormal cells may eventually develop into cancer cells, expand deeper into the cervix, and spread to nearby tissues.
Key Facts
- One of the biggest causes of cancer-related deaths among women is cervical cancer.
- Cervical cancer is the fourth most common disease in women worldwide, with an anticipated 604 000 new cases and 342 000 deaths in 2020.
- It has impacted young women at an increasing rate of 10% to 40% over the past 30 years.
- Around 90% of new cases and fatalities globally in 2020 took place in low- and middle-income nations.
- In 2022, it’s anticipated that more than 900 people were diagnosed with cervical cancer. The average patient is 49 years old when they were diagnosed.
- Nearly 50% of high grade cervical pre-cancers are caused by two human papilloma virus (HPV) types (16 and 18).
- Most of the people are infected with HPV mostly after the onset of sexual activity.
- Women living with HIV are 6 times more likely to develop cervical cancer compared to women without HIV.
Types of Cervical Cancer
These cancers are named for the type of cell that caused them. There are two primary types:
1. Squamous cell carcinoma
- Squamous cell carcinomas account for up to 90% of cervical cancer cases.
- These malignancies originate in the ectocervix’s cells.
2. Adenocarcinoma
- In the glandular cells of the endocervix, cervical adenocarcinomas form.
- A rare form of cervical adenocarcinoma known as clear cell adenocarcinoma is also known as clear cell carcinoma or mesonephroma.
- Squamous cell carcinoma and adenocarcinoma characteristics can occasionally be found in cervical cancer.
- This is referred to as adenosquamous carcinoma or mixed cancer. Only very rarely can other cervix cells become cancer.
Causes
- Human Papilloma Virus is the most common cause of cervical cancer.
- HPV is a common virus that is passed from one person to another during sex.
- When healthy cervix-based cells experience DNA changes (mutations), the development of cervical cancer follows.
- The cells are instructed by the mutations to grow and reproduce uncontrollably.
- The accumulated abnormal cells produce a mass (tumor). Cancer cells can infect the tissues in the immediate area and can separate from a tumor to spread (metastasize) to other parts of the body.
- Although the exact cause is unknown, HPV is known to have a part.
- The majority of HPV-positive people do not go on to develop cancer. This means that whether or not cancer develops also depends on other factors, such as your environment or lifestyle decisions.
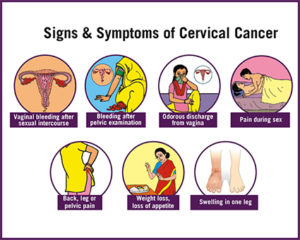
Symptoms
Cervical cancer alterations rarely result in symptoms. A cervical screening test is the only method to find out whether there are abnormal cells that could turn cancerous.
The following are the most typical symptoms if early cell alterations progress to cervical cancer:
- Bleeding after intercourse, between periods or after menopause
- Longer or heavier than usual menstrual bleeding
- Pain during sexual activity
- Bleeding following a sexual act
- Pelvic pain
- A change in your vaginal discharge, such as increased discharge or discharge that is visibly or odoratically different from normal
- Bleeding in the vagina after menopause.
As the cervical cancer advances, more complicated symptoms appear:
- Weight loss
- Fatigue
- Loss of appetite
- Continuous back pain, leg pain and pelvic pain
- Foul smell discharge
- Vaginal discomfort
- Swelling of leg/s or lower extremities
Risk Factors
- The main risk factor for cervical cancer, chronic infection with certain high-risk forms of the human papillomavirus (HPV), accounts for almost all occurrences of the disease.
- Smoking is the other major risk factor.
- Likelihood of contracting HPV increases with the number of sexual partners as well as the number of partners, the partner has.
- Early sexual activity: HPV risk is increased by having intercourse at a young age
- Additional sexually transmitted diseases (STIs): Currently if there is any other STIs such as Chlamydia, gonorrhea, syphilis, or HIV/AIDS, there is increased risk of cervical cancer
- Weak immune system: HPV can reduce immune system and if it is already compromised due to another medical issue, there is more likely to develop this cancer.
- Exposure to the miscarriage prevention medicine diethylstilbestrol (DES) is associated with a higher risk of developing the cervical cancer subtype known as clear cell adenocarcinoma.
Diagnosis
- A colposcopy shows the location and appearance of abnormal cells in the cervix, and a biopsy determines whether or not they are malignant.
- Screening aims to identify cellular alterations before they progress to malignancy. Since women have begun receiving routine screenings, the incidence of cases and fatalities from the disease has considerably declined.
- Pap test: This test finds irregular or abnormal cervix cells.
- HPV test: This test finds high-risk HPV infections, which are the ones most likely to result in cervical cancer.
Complications
- Complications can range from relatively modest ones, like minor vaginal bleeding or needing to urinate frequently, to life-threatening ones, such severe hemorrhage or renal failure.
Prevention
Generally, prevention of cervical cancer includes:
- Receiving vaccination to prevent HPV vaccination
- Having routine Pap tests: helps to detect precancerous condition of the cervix
- Practicing safe sex: Using condom during sex and limiting the number of sexual partners
- Stop smoking
Moreover, prevention can also be categorized as primary, secondary and tertiary prevention:
Primary prevention
- HPV vaccination for girls of 9-14 years of age
- Appropriate health information and awareness regarding the use of tobacco
- Sex education and condom promotion for those engaged in sexual activity
Secondary prevention
- Screening with a high performance test equivalent or better than HPV test
- Immediate treatment if the HPV molecular positive test
Tertiary prevention
Treatment of invasive cancer at any age:
- Surgery
- Radiotherapy
- Chemotherapy
- Palliative care
Treatment
- The disease’s stage affects how it is treated. Treatment for early and non-bulky disease (less than 4cm) includes surgery, occasionally followed by chemo radiation therapy.
- A cone biopsy may be sufficient to diagnose a tiny tumor; however, in rare instances, a hysterectomy—the surgical removal of the uterus—is necessary.
- A combination of chemotherapy (cisplatin) and radiation therapy (radiotherapy) is utilized for locally advanced illness.
- Treatment options for metastatic illness include palliative care only or chemotherapy (platinum/fluorouracil).
WHO Response
- The global strategy to hasten the eradication of cervical cancer as a public health issue was embraced by the World Health Assembly.
- The definition of cervical cancer elimination has been established as a country achieving a level of less than four cases of cervical cancer per 100,000 women annually.
- In order to attain this benchmark by the close of the 21st century, the WHO has established the 90-70-90 targets, which must be achieved by 2030 and maintained thereafter.
- 90% of girls fully vaccinated with HPV vaccine by age 15;
- 70% of women are screened with a high-performance test by 35, and again by 45 years of age; and
- 90% of women identified with cervical disease receive treatment (90% of women with pre-cancer treated; 90% of women with invasive cancer managed).
References and For More Information
https://www.cancer.org.au/cancer-information/types-of-cancer/cervical-cancer
https://www.mayoclinic.org/diseases-conditions/cervical-cancer/symptoms-causes/syc-20352501
https://www.cancer.gov/types/cervical
https://www.who.int/news-room/fact-sheets/detail/cervical-cancer
https://www.nhs.uk/conditions/cervical-cancer/
https://www.cdc.gov/cancer/cervical/basic_info/index.htm
https://www.cdc.gov/cancer/cervical/basic_info/risk_factors.htm
https://my.clevelandclinic.org/health/diseases/12216-cervical-cancer
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7797226/
https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0261503#sec001
https://www.statpearls.com/ArticleLibrary/viewarticle/19222