This content is also available in:
Italiano
Português
Deutsch
Čeština
Română
Türkçe
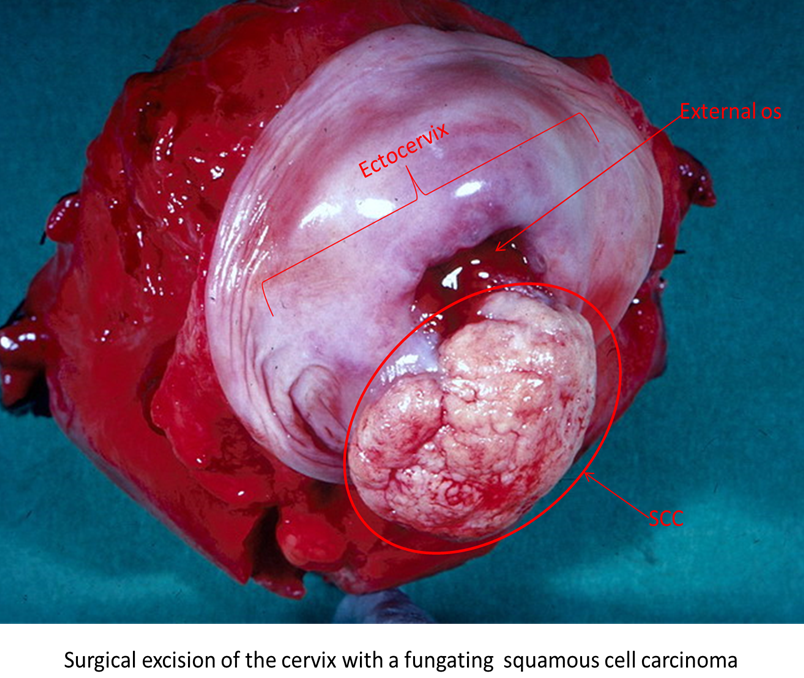
The clinical presentation and pattern of growth of invasive cervical cancer is variable. The tumour may be polypoid, papillomatous or fungating, or it may be flat or ulcerating (Figure 4.7). Initially, like most cancers, there is local spread or growth; it travels upward into the body of the uterus, downward into the vagina or laterally into the pelvic folds. Eventually the tumour may involve adjacent organs such as the bladder or rectum and eventual metastatic spread to the liver and other distant organs can occur. Involvement of the pelvic lymph nodes occurs early in the disease and is associated with a poor prognosis.
Cervical cancer is most commonly diagnosed in women aged 45-65, however they can occur in very young women (Austin & Zhao 2012). More screen-detected cancers are being diagnosed at an early stage due to the robustness of the cervical screening programme, clinicians requesting further investigations where younger women are presenting with clinical symptoms, and the introduction of HPV testing on cervical smears that morphologically appear only as low-grade lesions. Women with invasive cervical cancer are often asymptomatic in the early stage of the disease; they may present with post coital, intermenstrual, or post-menopausal bleeding. Backache or haematuria are presentations of when the tumour is at an advanced stage.
Stages of invasive cervical cancer
There are five clinical stages of carcinoma of the cervix described by the International Federation of Obstetrics and Gynaecology (FIGO) as shown below in Figure 4.8. The FIGO staging system is used by oncologists for planning treatment. The TNM system describes the tumour (T), lymph node involvement (N) and presence or absence of metastases (M) is used in histopathology reports.

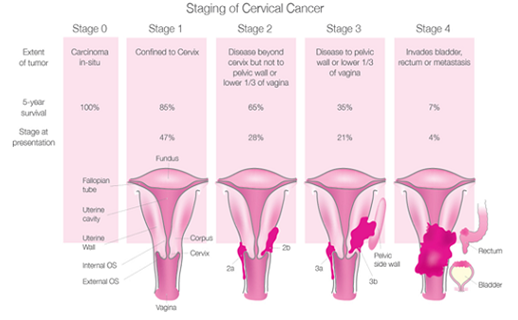
Stage 0 and Stage I comprise the preclinical stages of cervical carcinoma in which cervical screening and colposcopy play an important role in diagnosis as women are usually symptomless: the cancer is not visible with the naked eye and can be detected by cytology. Carcinoma in situ is now synonymous with CIN3 (stage 0).
- Stage IA carcinomas are known as microinvasive and are usually detected on cytology in asymptomatic women in the background of widespread CIN3.
- IA1 carcinomas are defined as invasion less than 3mm in depth or 7mm width; the smallest lesions are described as early stromal invasion.
- IA2 carcinomas are between 3 and 5mm in depth and less than 7mm in width; these carry a slightly higher risk of lymph node involvement.
- Stage IB1 cancers may either be symptomatic or asymptomatic and detected by screening (Andrea et al. 2012; Herbert et al. 2010).
Stages IB2 (more than 4-cm), II, III and IV are usually associated with clinical symptoms such as post-menopausal or post coital bleeding and comprise the clinically invasive stage of the disease
Survival is directly related to stage. Five-year survival is 100% for stage 0, 85% for stage I, 65% for stage II, 35% for stage III and 7% for stage IV.
- Among stage I cancers survival is higher for IA (approaching 100%) than IB (fully invasive) carcinomas
Treatment of cervical carcinoma
Treatment of cervical cancer is dependent on many factors. The main outcome for any cancer treatment is to preserve life and remove the tumour as quick as possible. However, patients diagnosed at a young age may still want to have children, which is taken into consideration when planning treatment.
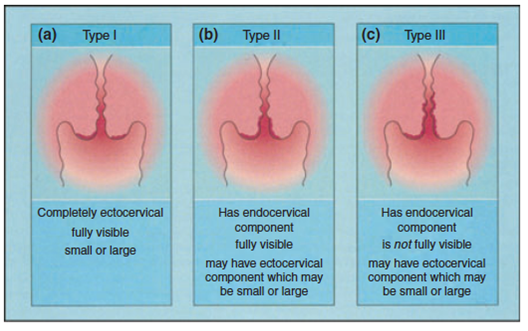
Carcinoma in situ/CIN3 (Stage 0) requires local ablation or excision of the lesion and the transformation zone (TZ) of the cervix, either by diathermy, laser, large loop excision of the TZ or knife cone biopsy depending its size and location on the cervix (Figure 5.10) (Jordan et al. 2008; Prendiville 2009).
Stage IA1 cancers may be treated by knife cone biopsy if the whole lesion and surrounding CIN3 can be completely excised.
Trachelectomy, or complete removal of the cervix, may be carried out for stage IA2 or IB1 cancers less than 2cm in size as a fertility saving treatment.
Stage IB cancers are usually treated by radical hysterectomy with or without preservation of the ovaries according to the patients age.
The standard treatments for advanced cervical cancer are radical hysterectomy and/or pelvic radiotherapy. More advanced cancers may require radiotherapy and /or chemotherapy. The clinical stage at time of diagnosis also affects the prognosis for the patient.
Histological types of cervical cancer
The World Health Organisation (WHO) recognises two main histological types of invasive cancer (WHO)
- Squamous carcinoma (which constitute about 85% of all cases)
- Adenocarcinoma (which constitute about 10-15% of all cases)
Other types of carcinoma include adenosquamous carcinomas, adenoid cystic carcinoma, neuroendocrine tumours, mesenchymal tumours, mixed epithelial/mesenchymal tumours and metastatic carcinoma make up the remaining 3-5% of all cases.
Learning points from Chapter 4
|

