Visceral Screening: An Important Aspect of Direct Access


Visceral Screening: An Important Aspect of Direct Access
If you are a primary care provider in any healthcare discipline, you need to have an awareness of visceral screening. This is important to identify co-morbidities as well as potential problems beyond your scope of practice.
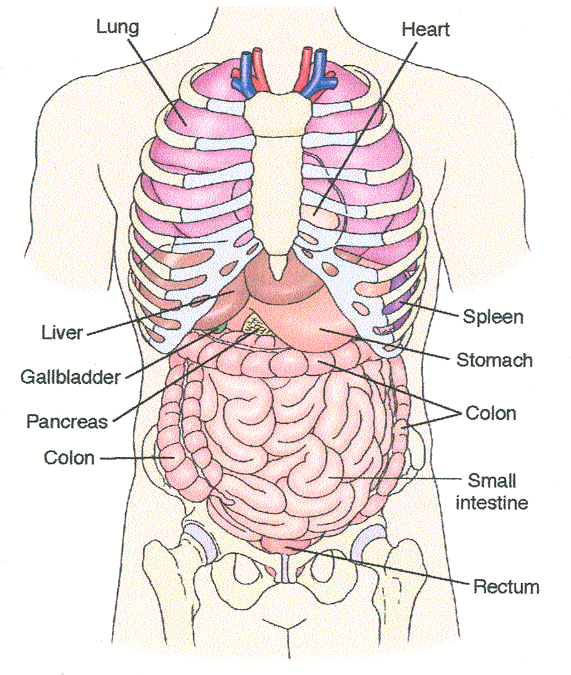
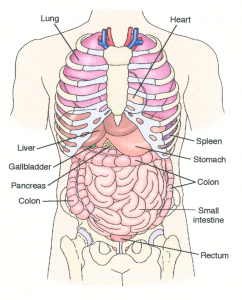
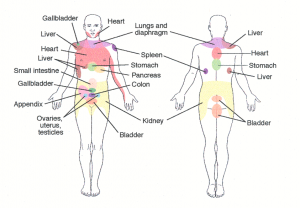
Visceral screening often includes reference to “red flags.” These are signs or symptoms that are strong predictors of pathology. The diagrams below show the anatomic location of the visceral structures and the referral pattern of each structure. When a patient reports right shoulder pain, it is important to rule out issues with the liver and gallbladder. Likewise, if an individual presents with hip or groin pain, the pathology could be originating from the kidney, bladder or colon, as well as the ovaries, uterus, or testicles. Furthermore, pain in the right lower quadrant may be from the appendix. Inquiring about these signs and symptoms in the medical interview and exploring the pain patterns are prudent.
 This blog is going to discuss the clinical tests used to detect visceral pathology. Let’s start with the Blumberg’s sign, known as rebound tenderness. This is a generic abdominal test which tells you if there is a problem with inflammation in the abdominal cavity. The technique involves pushing down vertically into the gut very slowly, and then releasing quickly. If the client reports discomfort upon release, that would be a positive test. However, a positive test does not tell you anything about what kind of problem may be present. It simply informs of the presence of an abdominal concern.
This blog is going to discuss the clinical tests used to detect visceral pathology. Let’s start with the Blumberg’s sign, known as rebound tenderness. This is a generic abdominal test which tells you if there is a problem with inflammation in the abdominal cavity. The technique involves pushing down vertically into the gut very slowly, and then releasing quickly. If the client reports discomfort upon release, that would be a positive test. However, a positive test does not tell you anything about what kind of problem may be present. It simply informs of the presence of an abdominal concern.
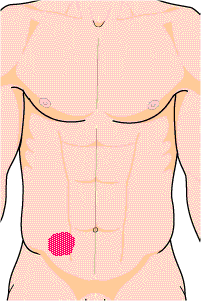 To specifically address some structures of the abdominal region, let us begin with the appendix. Many see the appendix as a structure of little value. However, the appendix is a reservoir for good bacteria. If you have ever had Montezuma’s Revenge, food poisoning, or taken a broad spectrum antibiotic that wiped out the good bacteria in your gut, the appendix is responsible for repopulating the good bacteria. Sometimes the appendix can become inflamed and palpation will reveal tenderness. Palpation of McBurney’s point can be helpful in pinpointing that condition. McBurney’s point is a location that is 1/3 of the distance between the anterior superior iliac spine (ASIS) and the umbilicus. If that spot is tender to palpation, it would be a positive test.
To specifically address some structures of the abdominal region, let us begin with the appendix. Many see the appendix as a structure of little value. However, the appendix is a reservoir for good bacteria. If you have ever had Montezuma’s Revenge, food poisoning, or taken a broad spectrum antibiotic that wiped out the good bacteria in your gut, the appendix is responsible for repopulating the good bacteria. Sometimes the appendix can become inflamed and palpation will reveal tenderness. Palpation of McBurney’s point can be helpful in pinpointing that condition. McBurney’s point is a location that is 1/3 of the distance between the anterior superior iliac spine (ASIS) and the umbilicus. If that spot is tender to palpation, it would be a positive test.
Two additional tests can be used for the appendix: psoas sign and obturator sign. The psoas sign capitalizes in the proximity of the psoas muscle to the 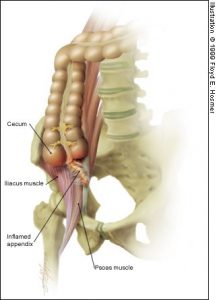 appendix. By incriminating the psoas muscle, an inflamed appendix will reproduce the pain. The test involves positioning the client in left sidelying and extending the right hip while stabilizing the lumbar spine. By taking the right hip back into
appendix. By incriminating the psoas muscle, an inflamed appendix will reproduce the pain. The test involves positioning the client in left sidelying and extending the right hip while stabilizing the lumbar spine. By taking the right hip back into  extension, the psoas muscle – a hip flexor- will tug on the adjacent appendix and reproduce the symptoms. That would be a positive test. Given that the specificity for this test is 95%, it can serve as a strong diagnostic tool. However, the clinician still must be certain that the client does not actually have a psoas injury. If there is any concern about the psoas test being a false positive, the obturator sign could be performed.
extension, the psoas muscle – a hip flexor- will tug on the adjacent appendix and reproduce the symptoms. That would be a positive test. Given that the specificity for this test is 95%, it can serve as a strong diagnostic tool. However, the clinician still must be certain that the client does not actually have a psoas injury. If there is any concern about the psoas test being a false positive, the obturator sign could be performed.
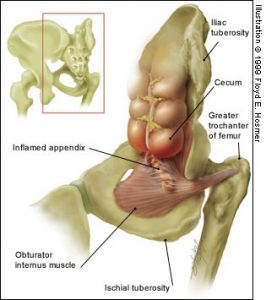 The obturator sign is similar to the psoas sign in that it uses the proximity of the obturator internus to the appendix as a means to incriminate the appendix.
The obturator sign is similar to the psoas sign in that it uses the proximity of the obturator internus to the appendix as a means to incriminate the appendix.  The test position is supine with the right hip and knee in 90° of flexion. The hip is then passively taken into internal rotation. Since the obturator internus is a hip external rotator, this position will put the muscle on a stretch and incriminate the appendix. Although in theory, the testing process parallels that of the psoas sign, there is not any statistical data to support its use.
The test position is supine with the right hip and knee in 90° of flexion. The hip is then passively taken into internal rotation. Since the obturator internus is a hip external rotator, this position will put the muscle on a stretch and incriminate the appendix. Although in theory, the testing process parallels that of the psoas sign, there is not any statistical data to support its use.
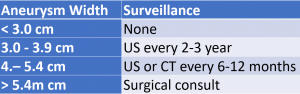
 Another structure worthy of screening is the abdominal aorta. Ruptured AAA is the 13th-leading cause of death in the United States (~15,000 deaths per year). The frequency of rupture is 4.4 cases per 100,000 persons. Palpation of the abdominal aorta width may be a helpful screening technique to identify this problem early. Palpation is performed in supine with the hips/knees flexed to relax the abdominal musculature. The clinician first identifies the xiphoid process and then the umbilicus. Go half way between these two structures just left of midline. Press firm and deep into the abdominal region to palpate the pulsation of the aorta (do not use the thumb to palpate). Once you find the lateral edge of the abdominal aorta on the right, find the lateral edge on the left. Place a thumb on one-side and an index/middle finger on the other side and measure this distance. This corresponds to the width of the abdominal aorta. A normal aortic pulse width is less than 2 cm (some literature says 3 cm). When accompanied by back pain with palpation and/or bruits on auscultation, reason for significant concern increases. This concern is evidenced by the statistics for this test:
Another structure worthy of screening is the abdominal aorta. Ruptured AAA is the 13th-leading cause of death in the United States (~15,000 deaths per year). The frequency of rupture is 4.4 cases per 100,000 persons. Palpation of the abdominal aorta width may be a helpful screening technique to identify this problem early. Palpation is performed in supine with the hips/knees flexed to relax the abdominal musculature. The clinician first identifies the xiphoid process and then the umbilicus. Go half way between these two structures just left of midline. Press firm and deep into the abdominal region to palpate the pulsation of the aorta (do not use the thumb to palpate). Once you find the lateral edge of the abdominal aorta on the right, find the lateral edge on the left. Place a thumb on one-side and an index/middle finger on the other side and measure this distance. This corresponds to the width of the abdominal aorta. A normal aortic pulse width is less than 2 cm (some literature says 3 cm). When accompanied by back pain with palpation and/or bruits on auscultation, reason for significant concern increases. This concern is evidenced by the statistics for this test:
Sensitivity = 31-77% & Specificity = 75-96%
(+) LR = 2.7-12.0 & (-) LR = 0.43-0.72
However, it is important to note sensitivity decreases significantly when abdominal girth exceeds 100cm (39.4 inches). The charts below reveal the recommended course of action when an AAA is suspected. 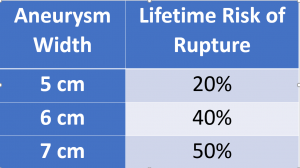
In addition to visceral palpation, there are other “red flags.” A number of indicators known as constitutional symptoms can be warnings of systemic pathology. These include signs and symptoms such as weight loss, fever, chills, pallor, bowel and bladder changes. None of these indicators are common with a musculoskeletal pathology. These are systemic concerns and suggest a deeper dive is in order.
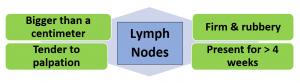
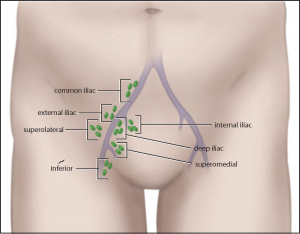 Finally, any time we see enlarged lymph nodes, we need to consider systemic issues. There are over 700 lymph nodes in our body. Axillary lymph nodes can easily be palpated. The location of the inguinal lymph nodes is displayed here. Upon palpation, if the lymph nodes are bigger than a centimeter, firm and rubbery, tender to palpation, and present for more the four weeks, the primary physician should be consulted.
Finally, any time we see enlarged lymph nodes, we need to consider systemic issues. There are over 700 lymph nodes in our body. Axillary lymph nodes can easily be palpated. The location of the inguinal lymph nodes is displayed here. Upon palpation, if the lymph nodes are bigger than a centimeter, firm and rubbery, tender to palpation, and present for more the four weeks, the primary physician should be consulted.
Consensus on what constitutes a red flag is slowly evolving in the literature (George, Beneciuk, Bialosky, Lentz, Zeppieri, Pei, & Wu, 2015). Red flags used in isolation may not be very informative. There is a lack of high-quality evidence for the diagnostic accuracy of many red flags. However, when used in combination with other aspects of the examination, they have value and could it instrumental in helping a person promptly access appropriate care.
 For videos of these techniques or more cutting-edge orthopedic information please subscribe to iOrtho+ Premium Web App. Prior blog posts and learning modules can be found at https://iortho.xyz/
For videos of these techniques or more cutting-edge orthopedic information please subscribe to iOrtho+ Premium Web App. Prior blog posts and learning modules can be found at https://iortho.xyz/
- George SZ, Beneciuk J, Bialosky JE, Lentz TA, Zeppieri G, Pei Q, & Wu SS. Development of a Review-of-Systems Screening Tool for Orthopaedic Physical Therapists: Results From the Optimal Screening for Prediction of Referral and Outcome (OSPRO) Cohort. JOSPT. 2015;45(7):512-526
- Gulick DT. iOrtho+ Mobile App. DTG Enterprises LLC. 2020
- Gulick, DT. OrthoNotes, 4th FA Davis Publishing, Philadelphia. 2018
