Reference Range
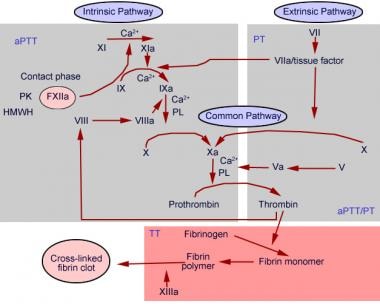
A basic understanding of the coagulation pathway is required to interpret prothrombin time (PT) result (see the image below). The prothrombin time is a measure of the integrity of the extrinsic and final common pathways of the coagulation cascade. This consists of tissue factor and factors VII, II (prothrombin), V, X, and fibrinogen. The test is performed by adding calcium and thromboplastin, an activator of the extrinsic pathway, to the blood sample then measuring the time (in seconds) required for fibrin clot formation.
Normal values include the following [1] :
-
The reference range for prothrombin time is 11.0-12.5 seconds; 85%-100% (although the normal range depends on reagents used for PT)
-
Full anticoagulant therapy: >1.5-2 times control value; 20%-30%
-
The reference range for the international normalized ratio (INR) is 0.8-1.1
Possible critical values are as follows [1] :
-
20 seconds
-
INR: >5.5
Interpretation
Various conditions may prolong or shorten prothrombin time.
Causes of prolonged PT include the following:
-
Warfarin use
-
Vitamin K deficiency from malnutrition, biliary obstruction, malabsorption syndromes, or use of antibiotics
-
Liver disease, due to diminished synthesis of clotting factors
-
Deficiency or presence of an inhibitor to factors VII, X, II/prothrombin, V, or fibrinogen
-
Disseminated intravascular coagulopathy (DIC)
-
Fibrinogen abnormality (eg, hypofibrinogenemia, afibrinogenemia, dysfibrinogenemia)
-
After bolus administration of heparin (PT may be transiently elevated)
-
Massive blood transfusion due to dilution of plasma clotting proteins
-
Hypothermia, as it causes inhibition of a series of enzymatic reactions of the coagulation cascade [2]
Causes of decreased PT include the following:
-
Vitamin K supplementation
-
Fresh frozen plasma transfusion
Collection and Panels
Drawing blood in a fasting state is not necessary, and no special preparations are required prior to the test.
The specimen used is whole blood obtained by routine venipuncture and collected in a blue-top tube containing 3.2% concentrated citrate.
One of the key components to the interpretation of prothrombin time is a properly collected sample. An adult sample tube with a volume of 5 mL must be filled completely or to at least 60-80% of its volume, as an incompletely filled tube may result in a falsely prolonged clotting time. [3] In addition, the sample must also be free of tissue fluids, intravenous fluids, heparin, or other solutions delivered through indwelling lines. Upon collection, the sample should be mixed gently by inversion 3 or 4 times and be tested within 2 hours if kept at room temperature (22-24ºC) or within 4 hours if kept cold (2-4ºC).
Background
A basic understanding of the coagulation pathway is required to interpret prothrombin time result (see the image below). The prothrombin time is a measure of the integrity of the extrinsic and final common pathways of the coagulation cascade. This consists of tissue factor and factors VII, II (prothrombin), V, X, and fibrinogen. The test is performed by adding calcium and thromboplastin, an activator of the extrinsic pathway, to the blood sample then measuring the time (in seconds) required for fibrin clot formation. [4]
In general, the prothrombin time is more sensitive to factor VII deficiency than factor deficiencies within the final common pathway. [5]
The prothrombin time has significant interlaboratory variability influenced by the instrument, and more importantly, the reagent used. In an effort to offset variation in thromboplastin reagent, and enhance standardization of PT in patients receiving warfarin, the World Health Organization (WHO) introduced the International normalized ratio (INR) in 1983. [6, 7, 8, 2, 9]
The INR is intended to standardize PT, such that a PT generated from one laboratory would yield an INR value comparable to that generated from any other laboratory in the world. [10] It is basically a mathematical conversion of a patient’s PT that accounts for the sensitivity of the reagent used in a given laboratory by factoring in the International Sensitivity Index (ISI) of assigned by its manufacturer. [5] The ISI is a measure of a reagent's sensitivity to a reduction in Vitamin K-dependent factors (II, VII, IX, X) compared with the WHO International Reference Preparation. The INR is then calculated using the following formula:
-
INR = [Patient PT/Mean PT]ISI
In this formula, patient PT is measured prothrombin time, mean PT is geometric mean PT of at least 20 healthy subjects of both sexes tested at a particular laboratory, and ISI is International Sensitivity Index that is specific to each reagent-instrument combination.
Considerations
The first step in evaluation of a prolonged PT and/or INR in a patient not on warfarin, without any history of blood dyscrasia and any medical problem that could explain an abnormal result, is to repeat the test to rule out a lab error. Various factors influence the prothrombin time and may result in falsely prolonged PT.
As mentioned, an adequate volume of blood is necessary for an accurate result. The volume of anticoagulant citrate in an adult tube is about 0.5 mL, and the intended ratio of whole blood to citrate is 9:1; hence, the tube must be filled completely or to at least 60-80%.
On the other hand, the recommended plasma-to-citrate ratio is 5:1. [5] Therefore, an elevated hematocrit, in conditions such as polycythemia vera, myelodysplastic syndromes, or cyanotic congenital heart disease, that results in a proportionate decrease in the plasma content of the sample relative to the citrate component may result in a falsely prolonged PT (dilution effect). In this instance, an appropriate amount of citrate, with the recommended plasma to citrate ratio of 5:1, should be added to the blood sample manually in a glass test tube.
A blood sample obtained after a bolus of heparin, from a site above heparin infusion, or through heparin-coated catheters may affect the PT. Heparin exerts its anticoagulant effect by inhibiting thrombin (factor II) of the final common pathway; hence, in theory it may prolong the PT. In order to offset this effect, heparin neutralizers are added to the thromboplastin reagent and can neutralize up to 2 U/mL of heparin. [5] Excess heparin, however, may overcome the ability of the neutralizing agent and prolong the PT.
Another factor that may cause an artifactual PT result is plasma turbidity. The current method of detecting clot formation is through an automated photo-optical method that records changes in light transmittance. As such, excess plasma turbidity in conditions like severe hyperlipidemia, hyperbilirubinemia, and hemolysis may cause artifactual PT results.
Lastly, note that the INR is validated only for patients on warfarin, and some concern exists regarding the validity of using it to determine bleeding risk in patients with chronic liver disease. Progressive liver disease is associated with variable changes in coagulation factors, and the degree of prolongation of the PT or INR roughly predicts bleeding risk. [2, 11]
-
Prothrombin time chart.