Overview
The kidneys are paired retroperitoneal structures that are normally located between the transverse processes of T12-L3 vertebrae, with the left kidney typically somewhat more superior in position than the right. The upper poles are normally oriented more medially and posteriorly than the lower poles.
The kidneys serve important functions, including filtration and excretion of metabolic waste products (urea and ammonium); regulation of necessary electrolytes, fluid, and acid-base balance; and stimulation of red blood cell production. They also serve to regulate blood pressure via the renin-angiotensin-aldosterone system, controlling reabsorption of water and maintaining intravascular volume. The kidneys also reabsorb glucose and amino acids and have hormonal functions via erythropoietin, calcitriol, and vitamin D activation. [1]
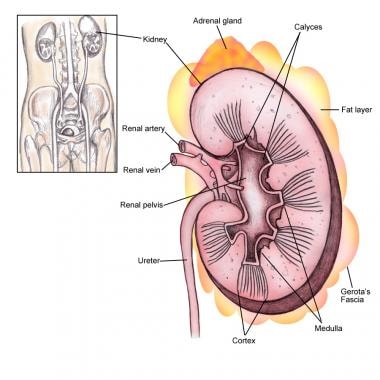
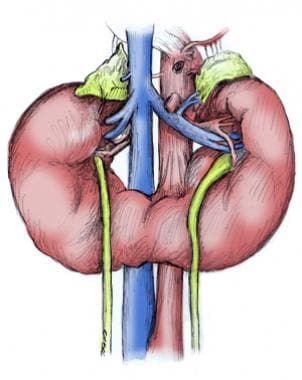
The kidney anatomy is shown in the image below.
Gross Anatomy
Grossly, the kidneys are bean-shaped structures and weigh about 150 g in the male and about 135 g in the female. They are typically 10-12 cm in length, 5-7 cm in width, and 2-3 cm in thickness. [2]
The relationship of neighboring organs to the kidneys is important, as described below:
-
Superiorly, the suprarenal (adrenal) glands sit adjacent to the upper pole of each kidney
-
On the right side, the second part of the duodenum (descending portion) abuts the medial aspect of the kidney
-
On the left side, the greater curvature of the stomach can drape over the superomedial aspect of the kidney, and the tail of the pancreas may extend to overlie the renal hilum
-
The spleen is located anterior to the upper pole and is connected by the splenorenal (lienorenal) ligaments
-
Inferiorly to these organs, the colon typically rests anteriorly to the kidneys on both sides
-
Posteriorly, the diaphragm covers the upper third of each kidney, with the 12th rib most commonly crossing the upper pole
-
The kidneys sit over the psoas (medially) and the quadratus lumborum muscles (laterally)
-
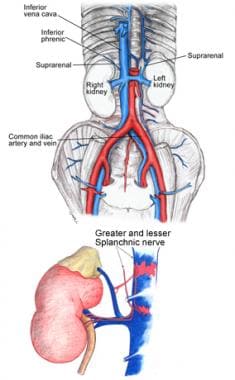
The images below further depict kidney anatomy and positioning
Vasculature
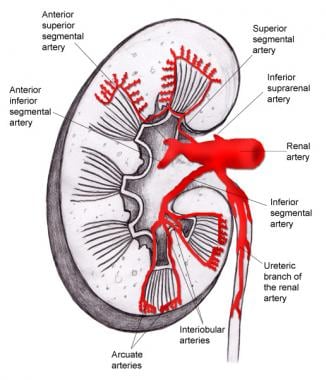
The kidneys receive approximately 20% of the cardiac output. The blood supply to the kidneys arises from the paired renal arteries at the level of L2. They enter into the renal hilum, the passageway into the kidney, with the renal vein anteriorly; the renal artery; and the renal pelvis posteriorly.
The first branch off of the renal artery is the inferior suprarenal artery. The renal artery then branches off into 5 segmental branches. The posterior segmental artery supplies most of the posterior kidney, with the exception of the lower pole. The anterior branches are the superior segmental artery, anterior superior segmental artery, anterior inferior segmental artery, and inferior segmental artery. These arteries branch into interlobar arteries, which travel in a parallel fashion in between the major calyces and then branch further into arcuate arteries that run within the cortex across the bases of the renal pyramids.
They then radiate into interlobular arteries, which extend into the cortex of the kidney to finally become afferent arterioles, then peritubular capillaries to efferent arterioles. Some of the terminal branches of the interlobular arteries become perforating radiate arteries, which supply the renal capsule. Renal pelvic and superior ureteric branches also originate from the renal artery and supply the upper portion of the collecting system (see the image below).
The renal veins drain the kidneys in a similar distribution, and the renal vein is generally anterior to the renal artery at the hilum. The left renal vein is longer than the right as it crosses the midline to reach the inferior vena cava (IVC). Generally, the left gonadal vein drains into the left renal vein inferiorly, while the left suprarenal vein drains into the superior aspect of the renal vein at approximately the same level. Posteriorly, the left second lumbar vein typically drains into the left renal vein as well. The left renal vein then crosses under the origin of the superior mesenteric artery to reach the IVC. On the right side, the renal vein and gonadal vein drain separately and directly into the IVC.
Renal Lymphatics
The lymphatic drainage parallels the venous drainage system. After leaving the renal hilum, the left primary lymphatic drainage is into the left lateral aortic lymph nodes, including nodes anterior and posterior to the aorta between the inferior mesenteric artery and the diaphragm. On the right, it drains into the right lateral caval lymph nodes. [3]
Collecting System
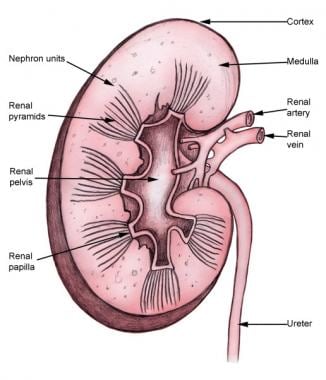
Once the filtrate gets to the collecting ducts in the medulla of the kidney, they converge to a renal papilla, which represents the tip or apex of the renal pyramid. Urine then collects in typically 9-12 minor calyces, which then converge into 3-4 major calyces (significant variation is possible).
The major calyces then empty into the renal pelvis, which passes urine through the ureteropelvic junction (UPJ) and into the ureter, which then propels urine distally to the bladder through peristalsis. The ureter may course posterior to the renal artery (or a lower pole branch) at its superior point, cross over the psoas muscle, and then pass posteriorly to the gonadal vessels. As it proceeds further distally, it passes over the iliac vessels and into the pelvis, finally traversing an intramural tunnel into the bladder and ending at the ureteral orifice on the trigone of the bladder (see the image below).
Renal Nerve Anatomy/Autonomic Innervation
The kidney receives autonomic supply via both the sympathetic and parasympathetic portions of the nervous system. The preganglionic sympathetic nervous innervation to the kidneys arises from the spinal cord at the level of T8-L1. They synapse onto the celiac and aorticorenal ganglia and follow the plexus of nerves that run with the arteries. Activation of the sympathetic system causes vasoconstriction of the renal vessels. Parasympathetic innervation arises from the 10th cranial nerve (X), the vagus nerve, and causes vasodilation when stimulated.
Microscopic Anatomy
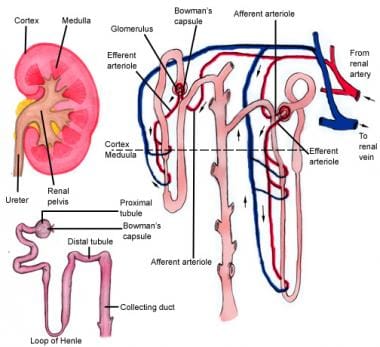
The kidney is divided into the cortex and medulla. Renal pyramids in the medullary areas are separated by the cortical tissue called renal columns (of Bertin).
Histology
The functional renal unit is the nephron, which is composed of the following:
-
The renal corpuscle: glomerulus and Bowman capsule
-
Proximal convoluted tubules (PCT, located in the renal cortex)
-
Descending loop of Henle (LOH)
-
Ascending limb (which resides in the renal medulla, leading to the thick ascending limb)
-
Thick ascending limb
-
Distal convoluted tubule
-
Collecting duct (which opens into the renal papilla)
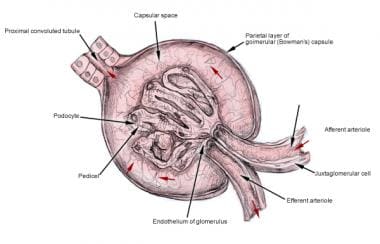
Blood from the afferent glomerular arteriole passes through the juxtamedullary apparatus to the glomerulus. The glomerulus is a network of capillaries that filters blood across Bowman capsule into the proximal convoluted tubule.
The glomerulus contains podocytes and a basement membrane allowing water and certain solutes to be filtered across. This filtrate then reaches the PCT, which reabsorbs glucose and various electrolytes along with water as the filtrate passes through. Meanwhile, after being filtered at the glomerulus, the blood passes into the efferent glomerular arteriole and then descends into the renal pyramid (see the images below).
Physiologic Considerations in Microscopic Anatomy
The renal tubular system is uniquely structured in order to maximize its physiologic function. One of its primary functions is to concentrate urine accordingly to the body’s hydro-osmotic state (either hyperosmotic or hypo-osmotic). A hyperosmotic state results in the excretion of hyperosmotic urine, and the reverse is true for when the body is in a hypo-osmotic state. The kidney is able to carry out this function by 2 mechanisms: the action of antidiuretic hormone on the medullary collecting ducts and the phenomenon termed countercurrent multiplication.
Countercurrent multiplication is responsible for keeping the medullary interstitial osmotic concentration higher than the renal tubular osmotic concentration. When the iso-osmotic fluid from the proximal tubule enters the descending limb, the osmotic concentration gradient forces water to move out of the descending limb. By the time the tubular fluid reaches the bottom of the loop of Henle, it has a higher osmotic concentration than the interstitial medullary fluid in the ascending limb. Hyperosmolar tubular fluid entering the ascending limb causes NaCl to be reabsorbed back into the medullary interstitium passively. Once the tubular fluid reaches the thick ascending limb, more ions are reabsorbed into the medullary interstitium actively.
The ion channel responsible for active transport in the thick ascending limb is the Na/K/2Cl transporter. The Na/K/2Cl active ion transporter is responsible for establishing a 200-mOsm/L concentration gradient between the tubular fluid and the interstitial fluid. The repetitive activity of active transport in the thick ascending limb, along with the passive reabsorption of NaCl in the ascending limb, adds more solute to the medulla in excess of water. This process causes a progressive increase in osmotic concentration from the corticomedullary junction (approximately 300-mOsm/L) into the deeper medullary interstitium (approximately 1200-mOsm/L). The elevated interstitial osmotic concentration helps concentrate urine entering the collecting tubules and ducts by increasing water reabsorption.
The vasa recti are a network of capillary vessels that mimic the structure of the loop of Henle. The main function of the vasa recti is to supply the renal medulla its metabolic needs while protecting the countercurrent exchange of the renal tubular system. This is accomplished by low medullary blood flow, allowing the renal medulla to receive the nutrients it needs while also preventing significant losses of solute from the medullary interstitium. In addition, the vasa recti have their own countercurrent exchange mechanism, preventing the washout of solutes from the medullary interstitium. [4]
Natural Variants
Anatomic variations in the renal vasculature occur in approximately 25-40% of patients. [2]
Supernumerary, or accessory, renal arteries are the most common arterial variation, with most of these branches supplying the lower pole of the kidney. They may pass anterior to the inferior vena cava (IVC) and over the ureteropelvic junction and be associated with (or cause) obstruction of the ureteropelvic junction (UPJ). Persistence of the right subcardinal vein anterior to the ureter can lead to a retrocaval ureter, which can also cause obstruction. [5]
The retro-aortic left renal vein (RLRV) is a malformation characterized by the presence of a vessel that drains the left renal blood up to the inferior vena cava crossing behind the aorta. The incidence varies between 1.7-2.5%, depending on series. It has surgical implications in renal surgery (ie, donor nephrectomy) more than clinical manifestations, although some authors have linked this to varicocele formation. [6]
Kidney position in the retroperitoneum is subject to variation as well. A kidney may be in an ectopic location, such as the pelvis, when it doesn’t ascend properly, or it can be malrotated or fused (as in horseshoe kidneys, in which the inferior poles are fused, causing a U-shaped configuration).
In some fusion anomalies, such as crossed-fused ectopia, the 2 kidneys may be located on the same side. Although some of these variations may be associated with pathological conditions, such as hydronephrosis and UPJ obstruction, they can also remain completely asymptomatic and undiscovered until a diagnosis is made by radiographic study.
Importantly, in an ectopic kidney, the adrenals should still be in the superior portion of the posterior peritoneum, since their embryologic origin is different from that of the kidneys.
Variants may also exist in the collecting system drainage. Duplication anomalies may develop, wherein more than a single collecting system may form and drain separately into the bladder (complete duplication) or join at some point proximally before draining into a single orifice into the urinary bladder (partial duplication). In a complete duplicated system, the upper pole moiety drains inferomedially into the bladder, and the lower pole moiety drains superolaterally, as described by the Weigert-Meyer rule. [7]
Pathophysiological Variants
Crossing Vessel, UPJ obstruction, Vesicoureteral Reflux
Crossing vessel, ureteropelvic junction (UPJ) obstruction, or vesicoureteral reflux can become pathophysiologic if it causes extrinsic or primary intrinsic obstruction leading to hydronephrosis. This can be seen with aberrant crossing vessels in a single system, which leads to UPJ obstruction. Obstruction can also occur from an ectopic ureter, where it is commonly seen inserting inferomedially in an abnormal location (ie, bladder neck) and is often associated with the upper pole moiety of a complete duplicated collecting system.
Similarly, a ureterocele in a single system, or sometimes seen in a complete duplicated system, can cause obstruction. From an intrinsic standpoint, UPJO can also be caused by an adynamic/aperistaltic segment of ureter that is due to abnormal embryologic development. Secondary etiologies of obstruction include stones, infections, iatrogenic ureteral damage causing strictures, and other acquired factors that are not due to anatomic variants.
Vesicoureteral reflux is another variation and is caused by an abnormal insertion of the ureter in the bladder in an abnormal position (usually superolateral). This insertion site leads to a shorter intramural tunnel length for the ureter to pass through the bladder wall, which leads to inadequate compression of the ureter during bladder filling and contraction and may allow reflux of urine up the ureter. Vesicoureteral reflux can contribute to pyelonephritis and, in extreme situations, irreversible damage to an affected renal unit.
The Nutcracker Syndrome
Anatomically, the Nutcracker syndrome involves the compression of the left renal vein between the aorta and superior mesenteric artery. Symptoms are nonspecific and include intermittent flank pain, microscopic hematuria, proteinuria, abdominal pain, and hypotension. Gynecological symptoms and varicoceles in the pelvis, buttocks, and thighs are also common manifestations.
Narrowing of the left renal vein on imaging studies is not enough to establish the diagnosis. Pressure gradient measurements between the left renal vein and inferior vena cava must be performed to confirm the diagnosis. Treatment is usually with endovascular stenting. [8]
Imaging Techniques for the Kidney
KUB (kidney, ureter, bladder) is the proper terminology for a radiograph of the abdomen when used to view the urinary tract. The outline of kidneys can usually be seen. Ureters usually are not visible. The most common pathological findings are urinary tract stones. [9] See the image below.
 Normal KUB (kidney, ureter, bladder) radiograph. Courtesy of Nevit Dilmen found at Wikimedia Commons.
Normal KUB (kidney, ureter, bladder) radiograph. Courtesy of Nevit Dilmen found at Wikimedia Commons.
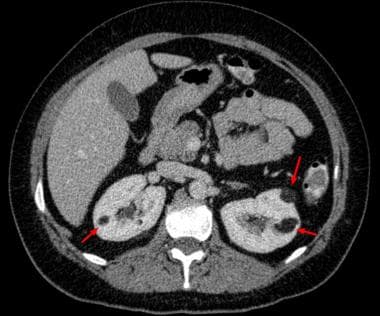
The imaging technique of choice for evaluation of the urinary tract and adrenal glands is CT scanning. It allows evaluation of the relative density of structures. CT scanning without contrast can be used for detection of renal or ureteral stones. [9] See the image below.
The advantages of ultrasonography include that it is readily available, does not require contrast, and avoids radiation exposure. The renal medulla is hypoechoic (darker) compared with the renal cortex. The renal cortex is isoechoic or slightly hypoechoic compared with the liver. Ultrasonography is able to identify simple or mildly complicated cysts and is able to differentiate these lesions from a solid mass. It is excellent for detecting hydronephrosis. [9] See the image below.
Radionuclide Renal Scintigraphy
Renal radionuclide imaging is an integral part of nuclear medicine and provides substantial information on the actual renal function.
The following radionuclides are used for dynamic imaging:
-
Tc-99m-diethylene triamine pentaacetic acid (DTPA) (Pentatate; 492 Da)
-
Tc-99m-MAG3 (Mertiatide; 350 Da)
For static imaging, Tc-99m-dimercaptosuccinic acid (DMSA) (Succimer; 281 Da) is used.
A diuretic challenge can also be administered.
DMSA scintigraphy includes assessment of renal size, identification of defects (eg, dilated calyces, scars) and a more precise measurement of differential renal function compared with other radionuclides. The use of a certain tracer depends on the clinical scenario and the diagnosis in question. Movement artifact and impaired renal function are pitfalls on test interpretation. Static scans are time consuming because of the long uptake and clearance of DMSA by the kidney; this is why MAG 3 scans are more commonly used.
Renal radionuclide scans are also used in the imaging of transplanted kidneys for such reasons as unexplained delayed graft function, complications like urine leak, or ureteral stenosis. [10] See the image below.
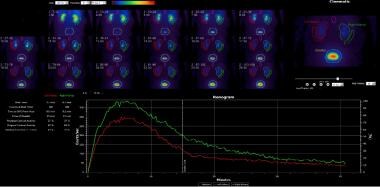 Images were obtained over the posterior renal region; 3.5 mCi of Tc-99m MAG3 was intravenously administered. Differential function was calculated. Postvoid images were obtained; 40 mg of Lasix was intravenously administered 15 minutes after administration of the radiopharmaceutical. Normal right and left renal uptake and transit and excretion is noted. The differential renal function is 57% right and 43% left. The right kidney appears slightly larger than the left, accounting for this differential function.
Images were obtained over the posterior renal region; 3.5 mCi of Tc-99m MAG3 was intravenously administered. Differential function was calculated. Postvoid images were obtained; 40 mg of Lasix was intravenously administered 15 minutes after administration of the radiopharmaceutical. Normal right and left renal uptake and transit and excretion is noted. The differential renal function is 57% right and 43% left. The right kidney appears slightly larger than the left, accounting for this differential function.
Surgical Considerations
Extraperitoneal Flank
When considering surgical approaches to the kidney, understanding the benefits, risks, and complications of each approach is paramount. The kidneys are retroperitoneal organs and, therefore, during an open surgery, one may choose to use an extraperitoneal flank approach, incising over the 11th-12th rib, plus or minus rib excision and staying retroperitoneally. This is particularly useful in obese patients, but not in patients with severe scoliosis or cardiorespiratory disorders, and provides direct access to the retroperitoneal space without traversing the peritoneal cavity.
Dorsal Lumbotomy
In the dorsal lumbotomy approach (which currently is rarely used in urologic surgery except in pediatric pyeloplasties for ureteropelvic junction repair), the patient is placed in a prone position, and a smaller muscle-sparing incision is made posteriorly without rib resection. It also provides a direct, retroperitoneal approach with a smaller incision but may be technically limiting in surgical exposure in larger patients and with differing pathology.
Transabdominal Approach
The transabdominal approach is performed with the patient lying supine and making either a subcostal or midline incision to traverse the peritoneum or reach the retroperitoneum. The renal pedicle is approached more directly using this technique, which is ideally suited to large and complex tumors or trauma, as the vessels can be approached quite proximally to establish early vascular control. Potential complications of the approach include postoperative ileus and future adhesion formation.
Thoracoabdominal Approach
The thoracoabdominal approach involves a lengthy incision over the chest wall and abdomen over the operative site. This approach is most often used for large tumors in radical nephrectomy, especially for those in the upper pole. Its disadvantages are increased pain and longer hospital stay and convalescence, as well as potential injury to the parietal pleura necessitating a thoracostomy tube. [11]
Laparoscopic Approach
From a minimally invasive perspective, laparoscopic and robotic-assisted laparoscopic approaches have been used for nearly all renal procedures, typically with reduced morbidity (primarily decreased postoperative pain and faster return to normal activity) when compared with open surgical techniques. Both transperitoneal and direct retroperitoneal approaches have been used and well described in the literature, and each has benefits and drawbacks to consider.
Laparoscopic procedures can be broken down into the following 3 categories:
-
Straight laparoscopic approach: In this laparoscopic approach, the surgeon does not use his or her hand. For transperitoneal laparoscopic renal surgery, 2 trocars are placed in the anterior axillary line—one half way between the anterior-superior iliac spine and the other trocar closer to the coastal margin. A third trocar site is placed in the abdominal midline, half way between the 2 trocars that were placed in the anterior axillary line. Trocar placement is essential for making the surgeon comfortable and enabling access of laparoscopic instruments to the surgical site.
-
Hand-assisted laparoscopic approach: This is a laparoscopic approach in which an additional incision is made for the surgeon’s nondominant hand. This enables palpation throughout the surgery in addition to the ability to retract and dissect by hand. Being able to feel surrounding organs and blood vessels serves the benefit of minimizing injury to vital structures.
-
Robot-assisted laparoscopic approach: This laparoscopic approach uses the Da Vinci surgical system and allows the surgeon to conduct the entire surgery from a console, which is equipped with robotic arms controlled from the console. The Da Vinci surgical system has expanded the scope of minimally invasive surgery, providing the surgeon with more comfort and precision throughout the procedure.
Percutaneous Approach
In percutaneous surgery, defining the calyceal anatomy is key. Patients are placed most commonly in the prone position, and direct entry into/through the retroperitoneal space allows access to the kidneys. For percutaneous stone surgery, access into the collecting system is performed under radiologic guidance. In other percutaneous procedures, such as thermoablation of small renal tumors, direct access to the site of pathology under real-time ultrasound or CT scan allows image-guided biopsy and treatment of lesions.
-
Renal anatomy, renal fascia.
-
Intrarenal arteries.
-
Microanatomy of the nephron.
-
Anatomy of collecting system.
-
Horseshoe kidney.
-
Kidneys.
-
Renal corpuscle.
-
Normal KUB (kidney, ureter, bladder) radiograph. Courtesy of Nevit Dilmen found at Wikimedia Commons.
-
CT scan showing angiomyolipoma of kidneys. Courtesy of Wikimedia Commons.
-
Normal ultrasound of right kidney. Courtesy of Wikimedia Commons.
-
Images were obtained over the posterior renal region; 3.5 mCi of Tc-99m MAG3 was intravenously administered. Differential function was calculated. Postvoid images were obtained; 40 mg of Lasix was intravenously administered 15 minutes after administration of the radiopharmaceutical. Normal right and left renal uptake and transit and excretion is noted. The differential renal function is 57% right and 43% left. The right kidney appears slightly larger than the left, accounting for this differential function.